Just as small, healthy habits create a foundation for long-term well-being — think a balanced diet, good night’s rest, regular exercise, and mindfulness — the same principle applies to the adoption of proactive, coordinated care. These foundational steps can feel overwhelming at first, especially if they’ve been neglected, but once established, they create momentum for positive change.
Similarly, building a culture of prevention and seamless care coordination begins with foundational shifts in mindset, operations, and technology. Like good habits leading to better health, the right strategies can lead to better outcomes, lower costs, and improved experiences across the entire care journey.
Are you prepared to lead this change without sacrificing the trust, engagement, and experience your members and patients depend on?
The integrated healthcare model seeks to achieve better patient outcomes and save costs through care that’s optimized across the spectrum of care providers with a focus on disease prevention/management of chronic conditions, rather than treatment of the disease and its complications.
At payer, provider, pharma, and manufacturing organizations, the drumbeat is getting louder to migrate toward care coordination. If you are the steward of customer experience (CX), guess what? Everyone’s looking at you for answers: How to shift to coordinated care, maintain the experience and better the health outcomes.
To help assess where you are on the continuum of readiness to shift to coordinated care, here are three questions to ask yourself:
Care coordination readiness — or not?
Question No. 1: Does my organization have the technological infrastructure to support care coordination, loosely defined as the organization of patient care across multiple healthcare providers? Adoption of electronic health records (EHRs) alone is not sufficient. Does my platform enable real-time sharing of patient health information across various healthcare settings?
Question No. 2: Is my organization culturally and operationally prepared to transition from volume-based to value-based care delivery? Has leadership committed to process changes, staff training, and new types of collaboration that prioritize and reward health outcomes?
Question No. 3: Does my organization possess in-house expertise to embark on the change management initiatives needed to support coordinated care? Have we investigated options to partner with third party experts to create, manage, and scale a coordinated care program? Have we identified a partner that’s easy to work with?
While 91% of primary care practices in the United States use EHRs, outpaced by the Netherlands, U.K., and other countries, there’s a big stretch of runway ahead before care coordination is realized and savings/efficiency achieved. EHR administration per patient visit (outside a typical 30-minute doctor’s appointment) averages 36 minutes, often after business hours dubbed “Pajama time,” and that leads to physician burnout.
Clearly, we can do better.
Relationships and CX that heals
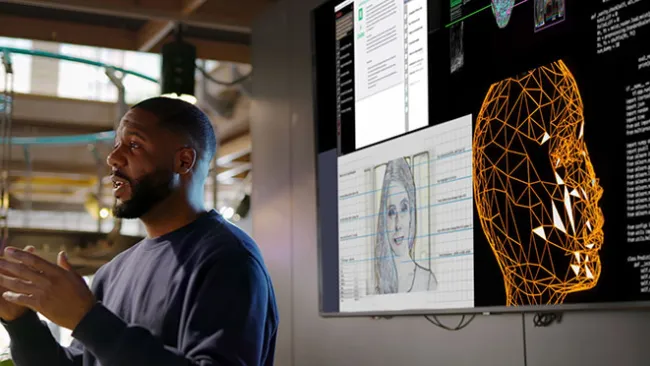
For inspiration, consider the strides made in coordinated care by one of our longtime clients, who we’ll call “Great Water Health” to safeguard their privacy. Through the use of AI, Great Water created a medical provider platform that assists with decision-making. The tool does not make decisions autonomously but rather assists the human clinician by offering machine learning-suggested testing, diagnoses, and treatment plans.
All this saves time a doctor might otherwise spend poring through medical records, freeing up the physician to spend more quality face time with patients. This ultimately leads to better health outcomes because patients are more engaged with their care and more likely to take ownership with medication adherence and preventative care.
More patients. Less paperwork. This point-of-care platform not only fosters stronger patient-physician relationships, but it results in fewer hospital admissions and emergency department visits because care is managed in a proactive manner.
Great Water Health’s unique and inclusive approach to healthcare — save costs and plunge profits back into lower-cost plans that reach more people — led to double-digit growth rates coupled with excellent patient outcomes.
Proactive outreach
TTEC supports Great Water in many ways to advance its care coordination mission while at the same time ensuring a quality patient/member experience at different stops along the healthcare journey:
- Take advantage! It’s not unusual for members to opt into coverage but fail to make use of it before the plan year ends. Take dental care. It’s well-established that oral health and general health are directly related and yet 21% of adults have at least one untreated cavity, according to the CDC. TTEC launched an outbound campaign for Great Water Health to remind members they still had time to take advantage of their health benefits and book a dental appointment, a friendly call nobody really expects but one that’s welcome when received.
- Follow-up is key: In another outbound campaign, TTEC reached out to call Great Water members who were just released from a hospital or inpatient facility to schedule follow-up care. Our healthcare advocates in the contact center offered members choices, such as an in-person visit with a nurse practitioner or a virtual visit — to ensure continuity of care.
- Provider assistance: Sometimes a member’s regular doctor disenrolls or is terminated from a payer’s plan, without notice. TTEC’s healthcare advocates contacted members who were patients of these providers to inform them their doctor is no longer in-network and to assist members in finding a well-qualified, new physician who is in-network and meets the member’s needs.
These examples represent just a handful of ways TTEC assists our clients on their journey toward full-scale care coordination. It’s all part of our mission to put humans at the center of healthcare. For a glimpse of how we see things shaping up in the next few years, check out 2028 Connected Healthcare.