Anyone encountering Folx Health for the first time will find the telehealth company’s mission as easy to understand as its pronunciation, “folks.”
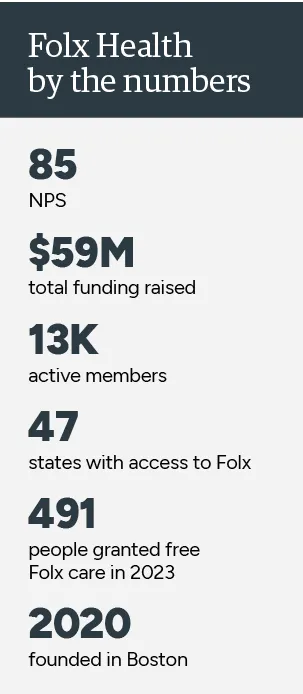
The Boston-based company delivers digital care designed for the LGBTQIA+ community via subscription-paid membership and as an employer benefit.
With a presence in 47 states, Folx provides virtual primary care and gender-affirming care along with educational resources, content, expert and peer support groups, plus care navigation that extends beyond the scope of telehealth. Folx mental health care is available in three states.
Kate Steinle, WHNP, Folx Health chief clinical officer, talked with Customer Strategist Journal about the impact Folx Health is having on its community and what’s coming in the near term.

In honor of Pride month and in partnership with The National Black Trans Advocacy Coalition, the Folx Care Fund will provide a free year of gender-affirming hormone therapy to 491 transgender people; that figure corresponds to the number of anti-LGBTQIA+ legislative bills in play today, according to Folx Health.
Customer Strategist: Some in the LGBTQIA+ community avoid healthcare for fear of discrimination or because they lack financial resources. Where does Folx Health come in?
Kate Steinle: We launched Folx Health in December 2020 with a focus on providing healthcare for the LGBTQIA+ community that is different from anything they have experienced. That means treating people as people instead of as problems to solve. A place where they feel seen and heard and therefore empowered. Joyful care comes out of that and people want to continue to be engaged with it.
We started with gender-affirming hormone therapy and have launched into sexual and reproductive healthcare. Mental health and primary care are the new areas we’ve moved into.
Anything that you can do through telehealth, we want to do better.
CS: Folx is strictly telehealth, offering care in a digital setting only?
KS: We also offer care navigation for anything outside the scope of telehealth.
If somebody needs in-person care for surgery or in-person care for cancer screenings, we have a national referral network of affirming providers and we direct our members right to them. We also have a community platform where our members connect with each other.
In care deserts, people often don’t have community and we wanted to create a content-rich, community-based platform where people can connect around support groups.
CS: What is your philosophy about the customer/patient experience? For those who’ve accessed telehealth on other platforms, what differences would they notice at Folx Health? Intake forms, for instance.
KS: They can see themselves centered in every question we ask. For example, we do not use gender terms such as “women’s” reproductive health. Instead, we frame our questions around the clinical need, such as: What type of birth control might you need based on your reproductive anatomy, or … for people with ovaries and a uterus.
That is the way we practice as clinicians: Make sure the question you are asking is clinically necessary, before you ask it. I want to make sure I’m recommending the best cancer screenings for your body parts. When we explain the reasons why we are asking a question, people are actually going to respond. And, they’re not going to feel concerned that you’re asking out of curiosity or may respond with disapproval or judgment.
CS: Folx has said it strives to deliver care that is not just affirming but also expert. What’s the distinction?
KS: Affirming care can be as simple as preferred pronoun stickers, imagery on your website or a pamphlet that’s representative of the community. It can be training, a commitment to treating this community. That’s all affirming. Patients feel like: OK, they got me. But some clinicians might not know the most recent studies, side effects. It’s a lot to keep up with the research. Patients expect an expert but they can’t always meet you there.
I don't mean to say affirming isn’t good. It is, but it’s not the pinnacle. Patients need an expert to drive their care forward in a different way than just somebody who’s kind of nice and affirming.
Expert is different. Expert is clinicians who have devoted their professional lives and careers to treating and understanding the health disparities of this community such as mental health conditions, higher rates of smoking, alcohol abuse, STIs, and heart disease. Experts are the ones presenting at conferences, doing the research and literature reviews to move protocols forward.
CS: In what other ways does Folx support the LGBTQIA+ community?
KS: It’s not just about the care we’re providing but we also offer support to those accessing care elsewhere and some clinicians, externally – education for the rest of the community. Our Library is accessible to anyone on the Internet. Our clinicians, community members, and writers produce articles that are pertinent to the lives and health of our community.
We build these articles specifically from what our community is asking us as clinicians.
CS: Do you see a role for artificial intelligence to better understand patients, personalize, and improve care?
KS: No question it will. We already use AI-powered things like Macros for charting, transcription of verbal medical notes recorded during patient visits.
That has an effect on patients’ coverage because insurance companies group things into rejected versus approved claims. We often have to bring up this exception because their systems are not built to recognize these exceptions.
CS: As chief clinical officer, what are your top priorities for the year ahead?
KS: We launched our mental health program about two months ago and we know that is a huge need for this community. We are in three states with that program, offering individual therapy and medication management. By the end of this year. I want to be in a lot more states. Our plan is to be across the country, but it takes time to license people and get the right people on staff.
Next month, we are launching primary care expansion for chronic disease management. That’s hypertension, diabetes, anything that we can do for primary care – making sure people know they can come to us not just for gender-affirming hormone care. They can come to us for everything.
We’re constantly working on improving the care delivery model from a clinician perspective and also from a patient perspective to make sure communication is as easy as possible.