The Centers for Medicare & Medicaid Services (CMS) Star Ratings system has always significantly impacted healthcare payers, influencing both consumer choices and financial returns, but its landscape is evolving. While clinical care quality and outcomes remain paramount, the role of customer experience (CX) is increasingly critical.
For 2026, CMS has introduced three new ratings measures:
- Kidney health evaluation for patients with diabetes
- Improving or maintaining physical health
- Improving or maintaining mental health
These measures will have growing importance in the coming years. Each one will carry a weight of one for 2026 but increase to a weight of three in 2027.
Investing in CX can help healthcare payers improve member experience, health outcomes, and Star Ratings for these new measures and across the board. By delivering positive CX fundamentals — timely access, clear communication, empathy, and proactive care — health plans can enhance both direct and indirect measures that contribute to higher Star Ratings.
Member experience in action: Mrs. Smith’s journey
To illustrate the impact of the new 2026 CMS Star Ratings measures, consider the journey of a hypothetical patient – Mrs. Smith, a 68-year-old Medicare Advantage member with diabetes-induced chronic kidney disease (CKD).
Though Mrs. Smith is fictional, her journey is representative of millions of Americans. By understanding her journey and her interactions with her Medicare Advantage plan, we can uncover key areas where targeted CX strategies can lead to improved ratings across millions of similar patient interactions.

CX can positively impact new measures
As the new measures take effect and impact payers’ star ratings, investing in high-quality CX – the right people, technology, and strategy – can set payers up for success.
When it comes to Mrs. Smith’s journey, for instance, here are ways the new measures could impact her (and millions of patients like her). Along with CX fundamentals, her payer should embrace technology to improve the member experience, become more efficient, and reap bottom-line benefits.
Kidney health evaluation for patients with diabetes
Patients like Mrs. Smith expect proactive scheduling for screenings and nephrology consults. Make things easier for them by automating preventive care reminders, ensuring healthcare advocates are trained to answer frequently asked questions, and prioritizing follow-ups for at-risk members.
When choosing technology to help, invest in AI-driven customer relationship management (CRM) tools for risk prediction and outreach automation, proactive scheduling for nephrology referrals, and dynamic knowledgebases that give associates real-time support.
Early detection of kidney disease progression, timely interventions, and treatment adherence can help improve member experience and outcomes and are essential for a higher star rating.
Improving or maintaining physical health
Mrs. Smith needs and expects smooth coordination among her primary and specialty care teams. Keep things moving seamlessly with a CRM-based health check reminder system that prompts healthcare advocates to follow up on adherence-to-care plans. Also, make sure associates have quick and easy access to wellness resources during interactions.
When it comes to technology, leverage integrated CRM with care coordination, wearable tracking, advanced analytics to close care gaps, telehealth solutions, and automated health check-in reminders.
These tools and can help payers prioritize preventive care and chronic disease management, and address social determinants of health, which can help improve their CMS ratings.
Improving or maintaining mental health
Her mental health is an important component of Mrs. Smith’s overall well-being; she’ll need routine mental health check-ins and easy access to counseling. Payers should eliminate guesswork by giving healthcare advocates a mental health checklist they can use to identify needs during calls. Then, make it easy for members to connect with mental health professionals when needed and automate monthly mental health check-ins for high-risk members.
The right technology can help here, too. Use AI-driven sentiment analysis to detect distress during member interactions, integrate telehealth-enabled mental health platforms, use dynamic scheduling to facilitate referrals scheduling, and equip associates with a centralized mental health knowledgebase.
In addition to improving members’ well-being, these steps will improve ratings since CMS expects health plans to demonstrate integrated mental and physical health care.
4 CX fundamentals that can drive results
Even with new CMS measures on the horizon, it’s still important for healthcare organizations to prioritize member experience. It remains a critical component of Star Ratings, not to mention a differentiator that gives payers a competitive advantage. Investing in CX fundamentals can help improve experiences, uncover efficiencies, and reduce costs.
But member experience remains a critical component of Star Ratings, not to mention a key differentiator that gives payers a competitive advantage. Embracing and investing in CX fundamentals can help organizations rise above the competition and improve members’ experiences while uncovering efficiencies and cost savings along the way.
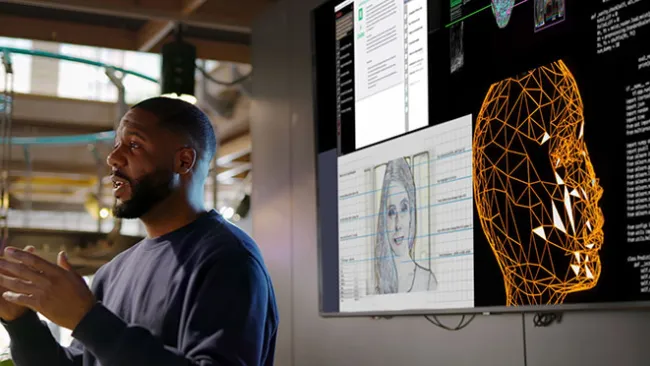
1. Real-time data and AI-driven insights
Why guess what’s delighting or frustrating members when you can know for certain? Having the right data collection and analytics tools are key to gauging member sentiment, assessing associate performance, identifying trends, and spotting roadblocks.
Traditional quality assurance tools typically evaluate fewer than 1% of associates’ interactions, giving companies little insight into how associates are performing.
Invest in tools like AI-enhanced quality and insights to listen to 100% of customer interactions in real time, uncover actionable trends, and make data-backed improvements. AI-powered insights also help pinpoint what skills and behaviors distinguish top-performing associates, allowing for targeted coaching that drives the greatest impact.
Strategy in action: When a nutrition supplements company sought to improve associate performance and customer engagement, we implemented AI-enhanced digital quality tools to analyze 100% of customer interactions. The results? Productivity jumped 97%, refunds decreased by 6%, resolution rates increased by 9%, and call volume dropped by 6%.
2. Empathetic, expert, and licensed associates
Equip front-line healthcare advocates with tools to manage interactions concerning chronic conditions compassionately and effectively. Training programs should focus on soft skills and empathetic communication, as well as condition-specific care protocols.
If in-house expertise is limited, partnering with a healthcare-focused outsourcing provider can offer access to a skilled labor pool. The right partner can bring AI-enhanced training solutions to onboard, train, and coach associates quickly and effectively, including when you need fast ramp-ups during the annual enrollment season.
Strategy in action: When a healthcare organization’s associates felt unprepared to confidently handle calls, we redesigned the company’s training and developed AI-enhanced conversational bots, leading to a 73% rise in skills practice time, a 4% increase in quality scores, a 4% increase in eNPS, and a 4% drop in call transfer rates.
3. Integrated health support with the right technology
Use a strategic blend of technologies –– from self-service tools to back-office solutions, to AI-enhanced learning and knowledge services –– to improve efficiency, satisfaction, and loyalty while meeting compliance and security needs.
With emerging AI tools like noise reduction, accent softening, and real-time translation, payers can deliver exceptional CX from nearly anywhere in the world without having to add headcounts.
Strategy in action: When associates and customers of a leading healthcare company struggled to understand each other due to background noises on both ends of the conversation, we deployed AI-enhanced noise reduction solutions within two weeks that led to a 99% reduction in audio issues and a 9% rise in NPS.
4. Automated, proactive outreach
Members expect a healthcare organization to not only meet their needs but also to anticipate them and reach out proactively. Evolving from a reactive to a proactive CX strategy can help improve member satisfaction and even prevent some member inquiries from ever reaching the contact center.
Use CRM automation to manage preventive care and appointment reminders, minimizing manual tracking. Expand solutions to include adherence to treatment plans, personalizing chronic care management, and supporting post-discharge care and wellness visits. This proactive approach builds reliability, reduces member stress, and drives higher satisfaction — all critical for Star Rating performance, while at the same time reducing call volumes at call centers.
At TTEC, we’ve seen these tools in action and the results they can drive. With 100% automated speech and text analytics, we deliver full intent mapping by connecting member intents, associate responses, and customer outcomes. Our intent-response-outcome (IRO) framework identifies high-impact drivers and focuses efforts where they matter most, improving business results.
Proactive CX insights from this approach have helped healthcare clients see a 3x reduction in associate churn through better information and support, 25% increase in CSAT by addressing key drivers of satisfaction, 5x faster QA evaluations, and 20% boost in efficiency through smarter resource allocation.
And in healthcare journeys, predictive model-based reminders and proactive outreach have been shown to reduce no-shows by as much as 11%, cut same-day cancellations by 6%, and significantly improve compliance with preventive screenings by up to 34%. The results? Better resource efficiency for organizations and better health outcomes for members.
Evolve with the future of healthcare CX
The 2026 CMS measures bring a new focus on proactive, holistic care. For health plans, now is the time to embrace CX fundamentals and the exciting new opportunities cutting-edge technologies bring.
If you lack the expertise in-house, working with a CX partner that specializes in healthcare is a great way to gain access to the labor pool, technology, and proven strategies needed to transform the member experience.
With the right blend of people and technology, payers can improve experiences and outcomes for millions of members like Mrs. Smith and drive Star Ratings success.