
Innovative call flow enhancements zap a major pain point
When a large regional payer struggled to increase health plan enrollments, TTEC replaced a traditional sales practice with a new call flow enhancement that delivered a better member experience and increased conversion rate
Innovative call flow enhancements zap a major pain point
When a large regional payer struggled to increase health plan enrollments, TTEC replaced a traditional sales practice with a new call flow enhancement that delivered a better member experience and increased conversion rate
sales conversion
compliance errors
The challenge
A common sales practice is to build value by telling customers about a product’s features before discussing the price. Sales associates for a large regional payer abided by this practice when selling health plans to prospective members. After presenting the plan, associates used the prospective member’s age, location, and family size to calculate a quote using the client’s enrollment system.
Many prospects felt frustrated going through a sales presentation only to discover that the price of the plan did not meet their budget. And since the plan costs were fixed, associates were unable to negotiate costs, leaving them with few solutions. The result was a sales process that negatively affected the caller experience for prospective members and employees.
Our solution
As a trusted partner, TTEC regularly identified opportunities to optimize the large regional payer’s member sales and support operations. We did it again by identifying and proposing a solution to the pricing pain point in the health plan enrollment process.
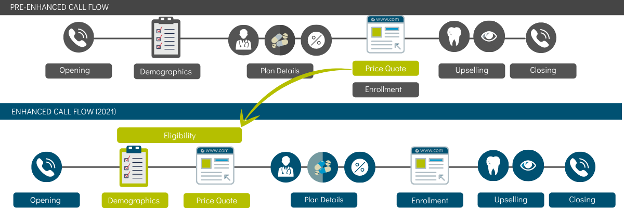
As part of a broader strategy to improve the call flow, we moved the cost discussion to the first part of the sales process, making it part of the eligibility discussion. After associates verified the caller's demographics, they provided a price quote up front. This way, associates offered appropriate responses to cost-related objections before moving to a more detailed discussion of the plan. This approach created a better member experience by ensuring the member's plan eligibility in terms of costs.
We also worked on aligning the associates’ KB resources with the client’s enrollment system. For instance, to verify a call, associates could quickly pull up a knowledge article reminding them to confirm demographic information such as the caller’s address and date of birth. Confirming the caller’s information is also the first step to create a price quote in the client’s system. Both the KB and the client’s system guide associates on the needed steps from the beginning until the end of the call. Whether the associate is reading their call scripts from the KB or entering information into the client’s system, compliance reminders and appropriate solutions are always available on their screens. By aligning the resources with the system, associates reduced compliance errors and provided better solutions.
The chart below shows the adjustments made to the call flow. The point at which an associate would provide a quote, for example, was moved up to the eligibility stage.
The results
As a result of TTEC’s proactive actions, peak sales conversion rates improved by 62%. Call accuracy, already high at 95%, increased an additional 2 percentage points to 97%. After implementing the new call flow, there were minimal to zero compliance errors as well.
And while implementing a new call flow often requires intensive up-training sessions, it was not necessary in this case. We improved the caller experience and increased sales conversion by including discussions regarding the call flow changes in the weekly team huddle and publishing KB banners — microlearning content — and team lead support to reinforce the use of the new call flow and provide the associates with consistent support. We continue to work with the client on implementing new solutions to improve the member experience and increase sales.












